Introduction:
Patients with congenital heart disease (CHD) are at increased risk of thromboembolism (TE) due to changes in blood flow, type of cardiac lesion, exposure to cardiopulmonary bypass, and cardiac catheterization. There are limited data describing the rate of and risk factors associated with recurrent TE in pediatric patients with CHD and prior TE. Therefore, the primary aim of this study was to describe the rate of recurrent TE in pediatric patients with CHD and a prior episode of TE. Secondary aims included: characterize the type of index and recurrent TE and site, as well as compare characteristics and risk factors of patients with CHD and history of index TE who developed recurrent TE versus to those who did not develop a recurrent TE.
Methods:
Patients in this study were enrolled and prospectively followed in the Johns Hopkins All Children's (St. Petersburg, FL) Institution-wide Prospective, Inception Multi-Cohort Study of Pediatric TE anytime between 2013 to present. For this analysis, patients were eligible for inclusion if they were <21 years of age, presented with an index TE, and had a diagnosis of CHD. Data collection included patient characteristics, clinical laboratory testing, radiologic results, type and site of TE, acute and chronic risk factors, and treatment agents. Frequencies/proportions were compared between groups by chi-squared or Fisher's exact test, as appropriate.
Results:
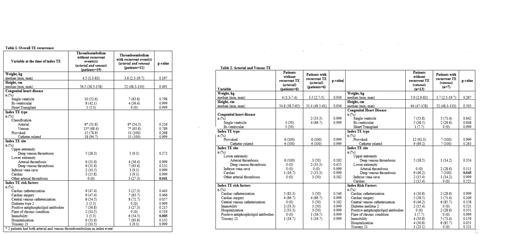
Thirty patients with CHD and index TE were included in this study. Of these, 11 (36.7%) patients had a total of 23 recurrent TEs. Five (45.5%) patients had one recurrent TE, 3 (27.3%) had two recurrent TEs, and another 3 patients had >2 recurrent TEs. Of the 23 recurrent TE, 3 events (13%) were arterial and 20 (87%) were venous. All 3 (100%) arterial TEs were provoked, and catheter related. Of the 20 venous TEs, 16 (80) were provoked and of these, 15 (93.8%) were catheter related. When compared to those who did not develop recurrent TE, patients who developed recurrent TE were more likely to have immobility (p=0.005), an arterial TE (p=0.041), or a lower extremity deep venous thrombosis (p=0.045) at the time of index TE. A greater proportion of patients with recurrence had a central catheter-associated TE compared to those with no recurrent TE but this difference was not statistically significant (73% vs 55%, p=0.057).
Conclusions:
In this single center prospective cohort we describe a high rate of recurrent TE (37%) among children with CHD and history of prior TE, and identified risk factors for TE recurrence. The vast majority of recurrent TE was provoked and catheter associated. Identified risk factors include immobility, and type and location of the index TE. Future multicenter prospective cohort studies are needed to validate these findings and identify additional risk factors.
Disclosures
Betensky:Janssen Pharmaceuticals: Consultancy, Honoraria. Goldenberg:Astra Zeneca: Consultancy; Bayer: Consultancy; Boehringer-Ingelheim: Consultancy; Chiesi: Consultancy; Novartis: Other: Data and Safety Monitoring Committee; Daiichi Sankyo: Consultancy; University of Colorado-affiliated Academic Research Organization CPC Clinical Research: Other: Serves on clinical trials oversite committees for pharma studies; Anthos Therapeutics: Consultancy.